Soon after cholesterol and fat start depositing on the lining of the blood vessels that supply your heart, the smooth muscle cells that give the blood vessels strength and flexibility start to get bigger and multiply.
While scientists studying the phenomenon suspect these vascular smooth muscle cells are trying to help, this atypical behavior for these strong cells instead contributes to coronary artery disease, the most common type of heart disease in the United States.
In a bit of a vicious cycle, stents as well as bypass grafts used to treat coronary artery disease can prompt the same response.
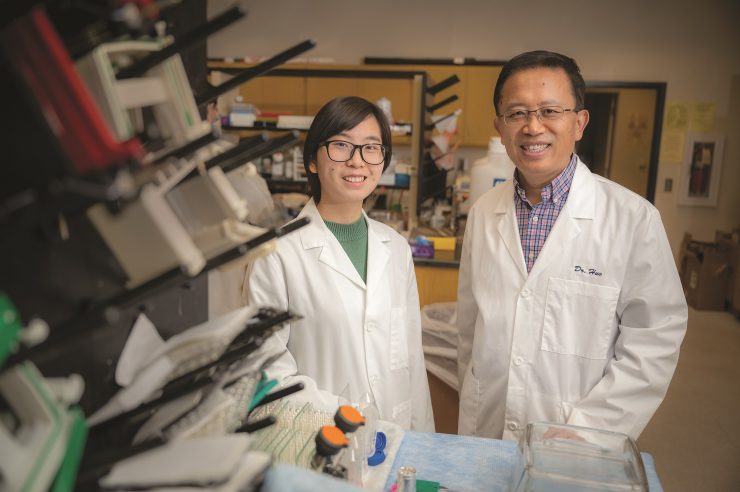
Now Medical College of Georgia scientists report new insight into how the cells enable this unhealthy growth and a new target to intervene.
The endothelial cells that line our blood vessels are in constant communication with the layers of vascular smooth muscle cells that encase them and play a key role in regulating our blood pressure, says Yuqing Huo, MD, PhD, director of the Vascular Inflammation Program in the Vascular Biology Center at MCG.
In states of good health, for example, the two cell types share messages about how it’s time for our blood vessels to dilate a little because we are exercising. Early in vascular disease, however the conversations change, says Huo, corresponding author of the study in the American Heart Association journal Circulation.
“They get the message that something is wrong,” says Huo, and existing cells get exponentially bigger and start proliferating, which these cells don’t normally do, perhaps in an effort to make more room inside for blood to flow since cholesterol and fat are narrowing the existing passageway.
“Normally the smooth muscle cells provide strength… if they start to proliferate a lot, it changes their identity,” Huo says.
Whatever the reason, the result is more narrowing and scarring of the vital passageway for blood and worsening disease. So, the scientists looked at the building blocks needed to enable the unhealthy response.
They knew that growing more and bigger cells requires more DNA, RNA and the proteins they produce. To make that happen requires more purines, one of two chemical compounds in the body used to make the building blocks of DNA, in this case adenine and guanine.
What they didn’t know was precisely how these cells make more purine when faced with arterial disease, says Qian Ma, PhD, postdoctoral fellow with Huo and the study’s first author.
There are two fundamental ways cells come up with purine: One is to essentially make it from scratch, called de novo purine synthesis, and the other is recycling.
The MCG scientists are the first to find that the higher-energy consuming de novo purine synthesis is increased in this scenario, Ma says. In the scar tissue and plaque inside blood vessels of mice and humans, Huo, Ma and their colleagues also found increased expression of ATIC, a gene essential to purine production.
“Our model demonstrates that this ATIC is important and targetable,” says Ma.
While there is still much work to do, Huo suspects an ATIC inhibitor would work best early in the disease process when an abnormal stress test indicates that cholesterol and fat in the blood are starting to deposit inside blood vessels and that applying an inhibitor to stents placed inside diseased blood vessels would be one good way to administer it.