The conversations between our bone and muscle change as we age, and both are the weaker for it, Medical College of Georgia scientists say.
They are leading a five-year, $11 million initiative funded by the National Institutes of Health to keep the conversation, our bone and muscle and ultimately us stronger longer.
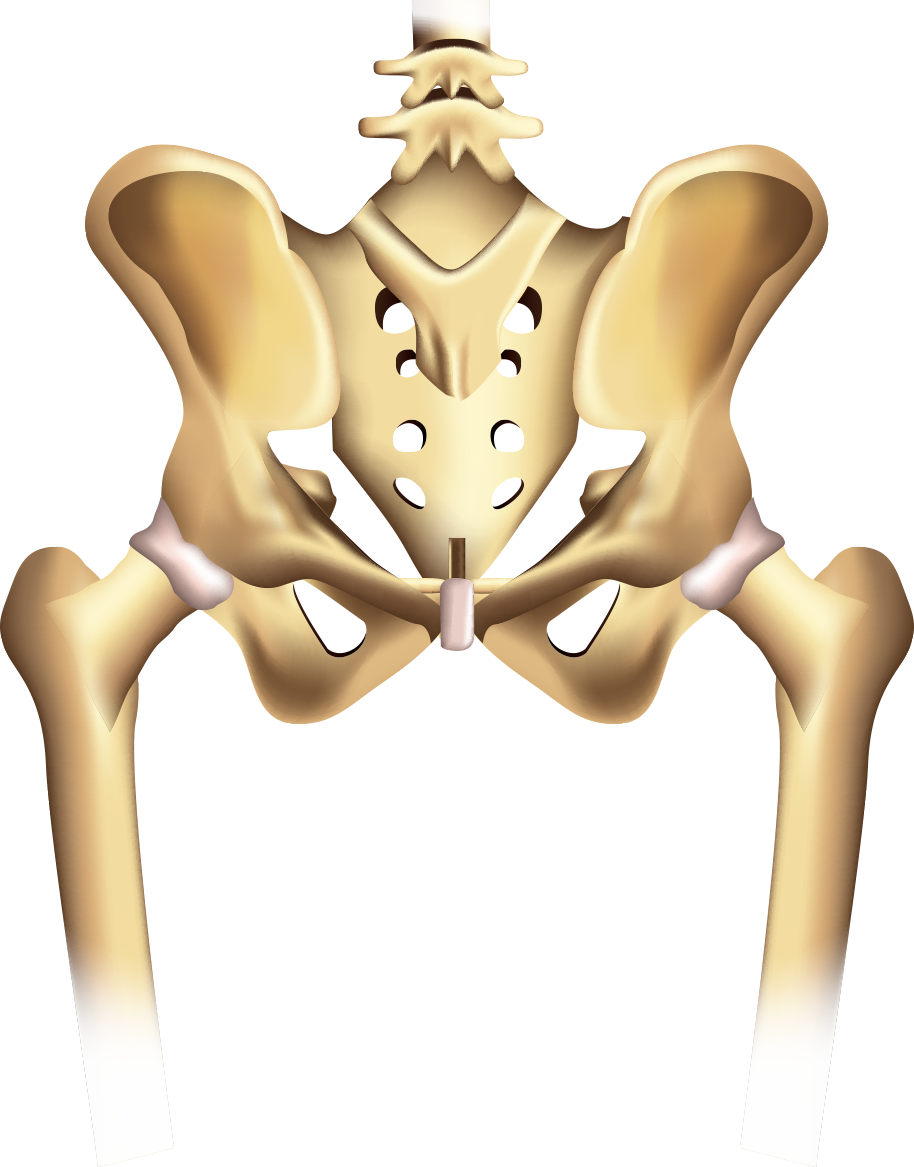
The bone and muscle that keep us upright are in constant communication and their wellbeing tends to go hand in hand, says Carlos Isales, MD, chief of the MCG Division of Endocrinology, Diabetes and Metabolism and co-director of the Center for Healthy Aging. Muscle loss, or sarcopenia, is a major cause of falls, and falls are a major cause of bone fractures, including common and potentially debilitating hip fractures.
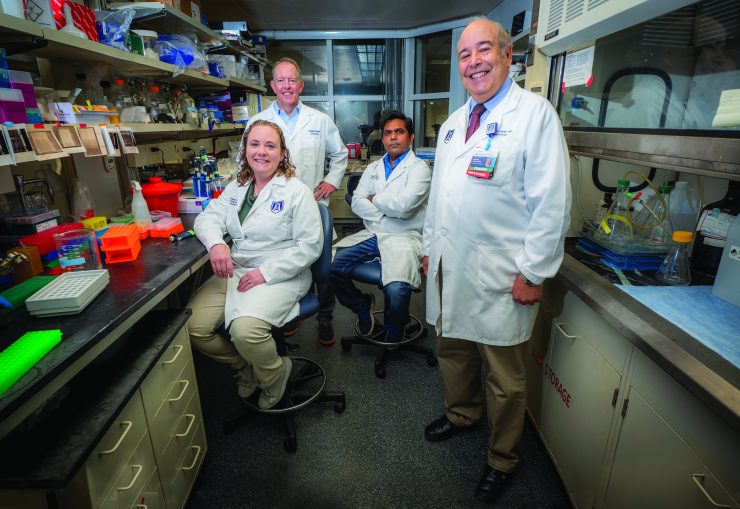
 Isales; Mark Hamrick, PhD, bone and muscle biologist and co-director of the Center for Healthy Aging; Sadanand Fulzele, PhD, aging researcher in the Department of Medicine; and Meghan McGee-Lawrence, PhD, a biomedical engineer in the Department of Cellular Biology and Anatomy, are principal investigators on the re-renewal of the NIH Program Project grant that will identify early, optimal points for novel interventions to change this dynamic in an aging population that is exploding with all 73 million baby boomers reaching age 65 by 2030.
Isales; Mark Hamrick, PhD, bone and muscle biologist and co-director of the Center for Healthy Aging; Sadanand Fulzele, PhD, aging researcher in the Department of Medicine; and Meghan McGee-Lawrence, PhD, a biomedical engineer in the Department of Cellular Biology and Anatomy, are principal investigators on the re-renewal of the NIH Program Project grant that will identify early, optimal points for novel interventions to change this dynamic in an aging population that is exploding with all 73 million baby boomers reaching age 65 by 2030.
Early in the complex biological dynamic than can go awry with age is tryptophan, an essential amino acid many of us associate with making us sleepy after a big turkey dinner. But Isales calls tryptophan “an important centerpiece of metabolism,” which helps us produce and maintain important proteins, enzymes even neurotransmitters that enable brain cells to communicate with each other and other cell types, like the constant communication between our brain and body so we can flex our muscles and move our legs.
Throughout life, the natural enzyme, indoleamine 2,3-dioxygenase 1, likely better known for its role in tamping down inflammation, breaks tryptophan down into usable products like kynurenine and picolinic acid, which are known to have an important role in the production of fuel for our cell powerhouses, or mitochondria.
But as with so many natural functions, with time the relationship becomes unbalanced. Our tryptophan levels tend to drop, while levels of IDO1 tend to rise.
Higher IDO1 levels mean more of the available tryptophan gets converted to kynurenine, which is now more likely to hook up with the aryl hydrocarbon receptor, or AhR, already associated with stiff, aging blood vessels in mice and humans. This connection means kynurenine instead damages cell powerhouses, increases inflammation and generally ages muscle and bone.
In bone and muscle, the MCG scientists say the receptor’s activation by kynurenine drives up destructive oxidative stress, which damages the powerhouses, which makes bone and muscle weak because cells don’t have the energy they need. “That is our idea,” Hamrick says.
“If we can prevent activation of AhR, we can prevent some of the bad things we have seen happen downstream,” McGee-Lawrence says, noting the drugs they are using for these studies were designed to inhibit the receptor in cancer.
The bottom line could mean that treatment of bone might help restore the health of muscle and/or vice versa, by helping restore healthier conversations between the two, Hamrick says. In fact, a class of existing drugs called bisphosphonates, which hone in to bone and today are widely used to treat osteoporosis, might be a good mechanism to deliver additional, targeted treatment, he says.