Deep in the brain a group of large neurons produce a hormone which prompts our bodies to hold onto more fluid and increase blood pressure.
Scientists say these neurons play a critical role in enabling our bodies to maintain healthy homeostasis by using this skill set to efficiently eliminate the excessive salt we consume in an unhealthy meal.
But scientists at MCG and Georgia State University also say that the chronic high-salt diet most Americans consume can turn this system against us, resulting in hyperactivity of these neurons, continuing production of this hormone vasopressin, constriction of blood vessels and increasing our risk for common cardiometabolic diseases like high blood pressure and heart disease.
Americans consume can turn this system against us, resulting in hyperactivity of these neurons, continuing production of this hormone vasopressin, constriction of blood vessels and increasing our risk for common cardiometabolic diseases like high blood pressure and heart disease.
A $2.7 million multi-principal investigator grant from the National Institutes of Health is enabling the scientists to further explore this apparently novel way cardiometabolic diseases happen and identify new therapeutic targets for them.
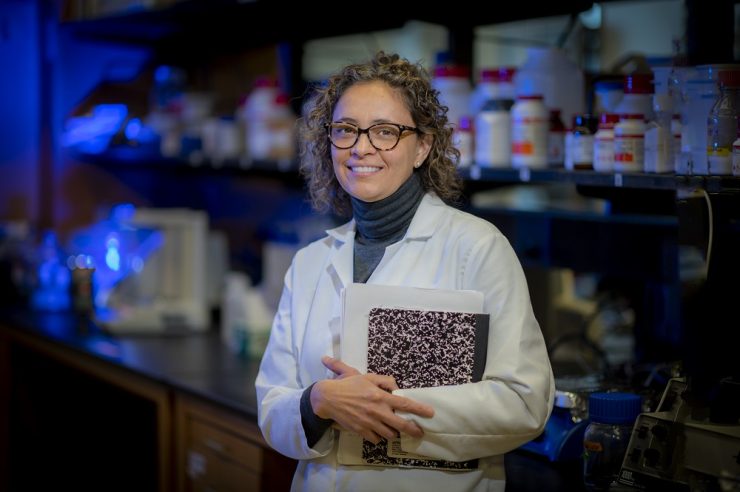
The large neurons in the supraoptic nucleus in the hypothalamus near the base of the brain secrete oxytocin, a hormone key to the reproductive system, as well as vasopressin, called an antidiuretic hormone because it actually helps the body hold onto fluids, which can help dilute excess salt in the body so it can be excreted in the urine, says Dr. Jessica A. Filosa, neurovascular physiologist in the MCG Department of Physiology.
She and Dr. Javier E. Stern, director of the GSU Center for Neuroinflammation and Cardiometabolic Diseases, are both PIs on the new grant.
They are finding that salt loading increases the firing of vasopressin-producing neurons, increases constriction of blood vessels and decreases local blood flow. More typically when neurons become active, blood flow to them increases, in a process called neurovascular coupling. This helps ensure working neurons have the adequate oxygen and nutrients needed to sustain increased activity.
In the supraoptic nucleus, however, Stern, Filosa and their colleagues, showed that the high activity of vasopressin neurons produces an apparently self-induced and sustained constriction of the vast network of blood vessels directly feeding them. The investigators also showed that the resulting local hypoxia — an oxygen supply considered inadequate to sustain homeostasis — was one of the mechanisms by which the activity of vasopressin neurons was further excited. It’s a form of inverse neurovascular coupling.
“Your body wants to stay in balance,” Filosa says. “Any time that you do something to your body or something happens to you that deviates from that balance, homeostatic processes turn on and (at least try) to restore balance.” In this case, excess salt is a trigger for the homeostatic processes.
But the process becomes a problem that instead contributes to high blood pressure and likely other problems when high-salt intake becomes chronic like it is for most of us: 90% of Americans age 2 and older consume too much sodium, according to the Centers for Disease Control and Prevention, an average of more than 3,400 milligrams daily compared to the recommended 2,300 milligrams.
The new grant is enabling studies in both tissue and an animal model Stern developed looking further at specific mechanisms and signaling and just how the resulting reduced blood flow in the region of vasopressin neurons manages to increase rather than decrease their activity. And, what happens to this unusual response in the face of conditions like heart failure.
They also want to know if they first constrict the blood vessels, does it still have this odd response of increasing neuron activity. This type of insight should help them better dissect the pathway. They already know that hypoxia makes the environment more acidic and that these neurons have an acid sensing ion channel, or ASIC, which means that a low pH can activate ASIC channels and increase the firing of the neurons. That could mean that chronic high salt consumption, which results in hypertension, vessel remodeling and enhanced constriction, also works in this direction to keep overstimulating the neurons to keep releasing vasopressin.
Another piece of the puzzle is astrocytes, those star-shaped brain cells that support neurons and typically step up their game when neurons are more active. But in this region, high salt intake prompts astrocytes to retract their processes which potentially worsens the scenario because one of the many jobs of astrocytes is to remove excitatory signals from where these neurons sit to keep them from overreacting.
They also are further exploring early evidence that yet another piece of the puzzle, the slow buildup of the natural, strong blood vessel dilator nitric oxide that hypoxia also induces, could be a mechanism for restoring homeostasis to these overactive neurons. There are multiple potential sources for nitric oxide nearby, including the neurons themselves, the supportive astrocytes, and potentially the endothelial cells that line blood vessels.