Our neurons and the glial cells that support them start showing up at about three weeks of gestation. The new neurons start producing chemicals and laying down fiber cabling so they can communicate with each other and with our bodies so we can function.
Never enough years later, deep in our brainstem, which helps keep our hearts beating and us breathing, these fundamental brain constituents are attacked in Alzheimer’s disease.
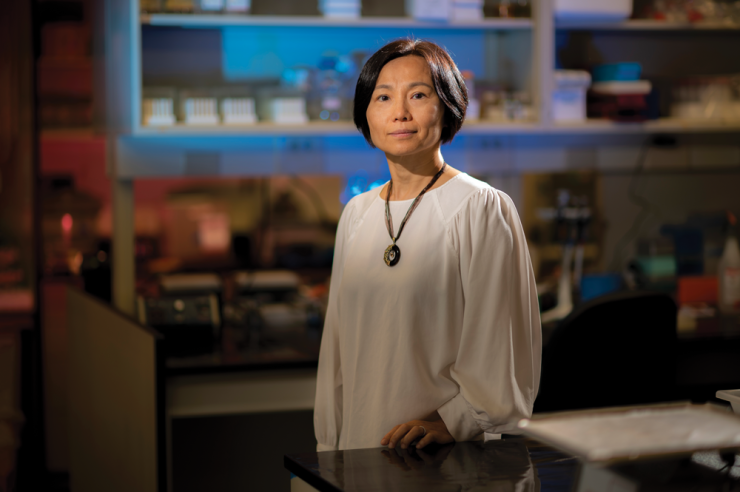
Dr. Qin Wang, neuropharmacologist, is combing the droves of investigational and approved drugs already out there for ones than can stop or at least slow this attack. The founding director of the Program for Alzheimer’s Therapeutics Discovery at the Medical College of Georgia is looking for the undiscovered power of existing drugs because it is a comparatively efficient approach, since the years of drug development and safety testing for humans already are done.
And, because there is a tsunami headed our way. An estimated 6.5 million Americans age 65 and older are now living with Alzheimer’s. Age is a primary risk factor, and the aging Baby Boomers are expected to nearly double that number by 2050, according to the Alzheimer’s Association.
She already has identified one drug, the investigational drug idazoxan, a small molecule that failed to receive Food and Drug Administration approval for depression. But it’s known to block the alpha 2A receptor in the noradrenergic system, famous for controlling our fight or flight response, which takes us back to the brainstem and the early damage Alzheimer’s causes.
Naturally curious
Wang was born for such pursuits. Growing up in a coastal city of Northeast China, she loved the beauty and the secrets of the expansive sea. It was not long after the end of China’s Cultural Revolution, during which schools were closed and the economy essentially shut down with them. But by the 1980s public education was good again and STEM was a focus. She would read biographies, like about her hero Madame Curie. “I wanted to be her,” says the intrinsically curious Wang. Her proud parents wanted her to be a physician, and in 1992 she graduated with honors from Peking University Health Sciences Center. There was no doubt that the world’s most populous country needed and still needs physicians. But it was in the research labs where Wang found the most inspiration and excitement and eventually the brain, one of our body’s biggest mysteries.
She came to the United States and the University of Iowa because the graduate programs in her homeland were frankly still not as good at that time. She found great science and good people. Despite having studied English for a dozen years in China, the language barrier was very real when she arrived in the Midwest, but so were the people who would take her to the post office, rather than just trying to tell her how to get there. At Iowa she would study transcriptional regulation, which is fundamentally the biological cues for, in this case, heart development, which like the brain begins as early as three weeks of gestation. Her mentor was the now Professor Emeritus Dr. Jung-Ching “Jim” Lin, who just a few years before Wang’s 1999 arrival in Iowa, had discovered Xin repeating containing proteins, which are key to healthy heart development. Lin had trained under a great scientist as well, Dr. James Watson, geneticist, biophysicist and Nobel Prize winner for his key role in discovering the molecular structure of DNA.
Wang opted to pursue postdoctoral studies in molecular pharmacology at Vanderbilt University in the lab of the energetic and inspirational Dr. Lee Limbird, who was studying G protein-coupled receptors. The receptor family is the largest protein family in our body. These receptors get made inside cells then move to the surface where they are important to a myriad of functions, like our sense of taste, and to regulating mood and our immune system. They also are a target for many of the existing medications Wang now studies. Limbird, Vanderbilt’s first associate vice chancellor for research who also chaired the Department of Pharmacology, also had studied with a Nobel Prize winner, Dr. Robert J. Lefkowitz, cardiologist and scientist, honored for his work in this big family of receptors.
Wang too found herself “immersed” in receptors, Limbird and a field in which, contrary to what non-pharmacologists might surmise, you typically have a drug before you really, if ever, completely understand how it works, including which receptor(s) it targets. Wang reminds you that for thousands of years, people used “medicines” without having a clue how they worked, maybe just because of anecdotes shared by a neighbor that they did. It wasn’t until the last decades of the 20th century that serious thought was given to which receptors (few target just one) drugs must be interacting with and the technical ability to look for those receptors emerged.
Receptive points of contact
Receptors are key communication points for our cells that exist as points of contact for innate body substances and often for more than one of these natural signaling molecules, or ligands. “These days we are still trying to figure out how they do different things, how we can manipulate that, how to block one pathway and keep another,” Wang says of multitasking receptors.
She is focused on the noradrenergic system, whose receptors regulate a ton of functions like sleep, mood and addiction and are critical for cognition. This system’s primary neurotransmitter is norepinephrine, or noradrenaline, made by neurons in the brainstem and which enables us to prepare for many things, including running from an assailant. This system is also an early target in Alzheimer’s.
While still at the University of Alabama at Birmingham, which she moved to in 2005, Wang and her colleagues put together new, twisted pieces that ultimately link noradrenaline to enhanced toxicity of the amyloid β and tau proteins that collect in the brain in Alzheimer’s.
They reported in early 2020 in the journal Science Translational Medicine that amyloid β molecules bind to one of the receptors in the noradrenergic system, that alpha 2A adrenergic receptor, to hijack norepinephrine signaling and redirect it to make a pathway for making changes to the tau protein that make tau toxic to the brain. Tau’s more usual function actually is to help stabilize the skeleton of our neurons. The binding also increases alpha 2A adrenergic receptor activity. This high expression of alpha 2A receptor in noradrenergic neurons in the brainstem is likely one reason that this area of the brain is so vulnerable in Alzheimer’s. Their findings held in animal models and in human brain tissue.
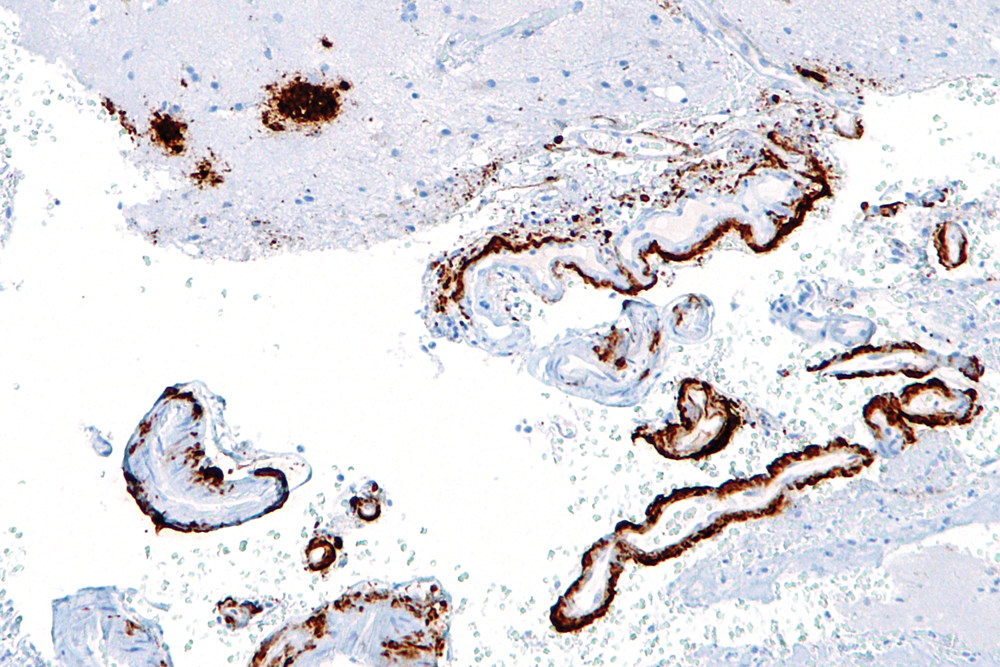
The scientists also used the National Alzheimer’s Coordinating Center database to look at individuals who took clonidine, a high blood pressure medication that activates the alpha 2A adrenergic receptor, and found that the drug’s use was associated with worsening cognitive decline in those with cognitive problems but didn’t affect the thinking of those without them. That helped confirm how hyperactivation of this receptor accelerated cognitive decline in patients.
Further, eight weeks of treatment with idazoxan, which blocks the alpha 2A adrenergic receptor, reversed aberrant activation of the detrimental signaling cascade and there was less amyloid β, less negative impact on tau and less brain inflammation.
In fact, mouse models treated with idazoxan, even with a lot of amyloid β present in the brain, acted similarly to their disease-free counterparts in maneuvering tasks that rely on a good memory. The scientists wrote then that combining a drug that blocks the receptor with one known to reduce amyloid β load could provide more benefit to patients.
“We found the results exciting because it rescued our mice,” Wang said. For example, in the hippocampus, the center of learning and memory, treatment resulted in more of those fibers that neurons send out that enable communication inside the brain being preserved. Conversely without treatment, brainstem projections were few in number in the hippocampus, a major warzone in the disease.
They gave the drug at different stages of the disease, and while early is almost always best with any therapy, they found that even later in the disease process, it helped stop further fiber degeneration. Perhaps as importantly, the mice functioned more normally. The research also provided more insight into why treatments that reduce, but don’t eliminate, amyloid β have not been more successful.
Wang, a Georgia Research Alliance Eminent Scholar in Neuropharmacology, joined the MCG faculty in April 2021 after being in Birmingham about 16 years. A primary reason to relocate was the Transdisciplinary Research initiative in Inflammaging and Brain Aging announced by Augusta University President Brooks Keel last year. Wang was the first new recruit as part of the three-year, $15 million initiative that includes MCG and the AU School of Computer and Cyber Sciences, Dental College of Georgia and colleges of Nursing, Allied Health Sciences and Science and Mathematics.
“I see the initiative as a platform to really boost Alzheimer’s research here,” she says. “This is a really complex disease that involves many other organ systems like the heart, and other conditions, such as having diabetes or needing cancer treatment, can increase the risk.”
“These days we are still trying to figure out how receptors do different things, and how we canmanipulate that to keep one pathway and block another…It’s really hard to develop central nervous system drugs because your brain keeps adapting,”– Dr. Qin Wang
Next steps
One of the many steps she is taking in her lab now and as lead of the Program for Alzheimer’s Therapeutics Discovery is clinical trials to see how/if the benefits of idazoxan translate to humans, as she suspects it will.
She is working with the biotech company that developed the drug to get trials underway as soon as possible. She also is working with them to potentially develop new drugs that are even more specific at blocking the deleterious role hyperactivation of the alpha 2A adrenergic receptor plays in Alzheimer’s. That means also learning more about the current target receptor while still looking for new targets. She also is looking more at those fibers and connectivity.
‘These days we are still trying to figure out how receptors do different things, and how we can manipulate that to keep one pathway and block another,” she says of the big challenges and big topics in her field.
But new drug development, always an arduous process, can be a particularly long, hard road in the brain, she says.
“It’s really hard to develop central nervous system drugs because your brain keeps adapting,” Wang says, and a drug’s constant stimulation of a receptor can eventually downregulate the targeted receptor, even cause it to disappear from the cell surface.
“That is just biology. They just don’t like that,” Wang says. It’s also what happens in Alzheimer’s as the early frenzied, almost seizure-like activity of neurons precedes their eventual slowing, loss of connectivity and death.
But those challenges do not deter Wang or her smile. Like most people, she has personally experienced the loss that Alzheimer’s brings as it steals away a person that you love and a great mind that you respected.
“I really want to see it, to solve it. It’s not hard to stay inspired, because there is just so much to learn and to do.”
Note: Dr. Qin Wang, a faculty member in the MCG Department of Neuroscience and Regenerative Medicine, is currently principal investigator on three National Institutes of Health grants and contact PI on two additional multi-PI NIH grants. She was among the top 20 out of 869 NIH-funded PIs in the nation’s anatomy/cell biology departments in 2020.
To donate to Dr. Wang’s work and the Department of Neuroscience and Regenerative Medicine, visit https://www.augusta.edu/mcg/dnrm/give-to-dnrm.php, call 706-721-4001 or email philanthropy@augusta.edu