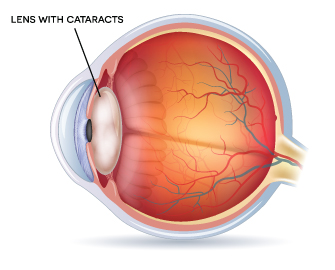
The crystalline lenses of our eyes are our intrinsic sunglasses.
Vitamin C, important to a host of essential functions like forming blood vessels and cartilage, enables the lens to do most of this important work of protecting our retinas from destructive ultraviolet radiation even without trendy shades.
But in one of many ironies, the high oxygen use required in this relentless task produces a lot of damaging byproduct, called reactive oxygen specifies, which can hurt vitamin C’s sunscreen skill. The natural, abundant antioxidant glutathione steps in, continuously converting vitamin C back to its natural state in a process that typically keeps our lenses clear for decades.
Meanwhile, over time, our glucose metabolism starts going sideways, so more of the sugar starts attaching to proteins, the main component of the lens, and making more damaging byproducts in the process. Also meanwhile, levels of glutathione, which detoxifies protein oxidation, are dropping.
This is all happening in a unique area of the body where protein just does not turn over. You keep the lens protein you are born with, at least until an ophthalmologist removes your lens and replaces it with a manmade one during cataract surgery. For comparison sake, red blood cells, which contain the oxygen-carrying protein hemoglobin, only survive about 120 days, and we make several million red blood cells every second.
Typically about age 50, this dynamic starts turning the crystalline lens a distinctive yellowish.
It’s called the Maillard reaction, discovered 110 years ago by a French scientist and the same chemical reaction that gives browned meats that distinctive flavor. But this is hardly tasteful.
More than the color of the protein gets changed and more bad stuff starts sticking to it and proteins start unnaturally sticking to each other. The way our skin becomes less elastic with age is a good example of what the unnatural connection does to the protein. It stiffens up.
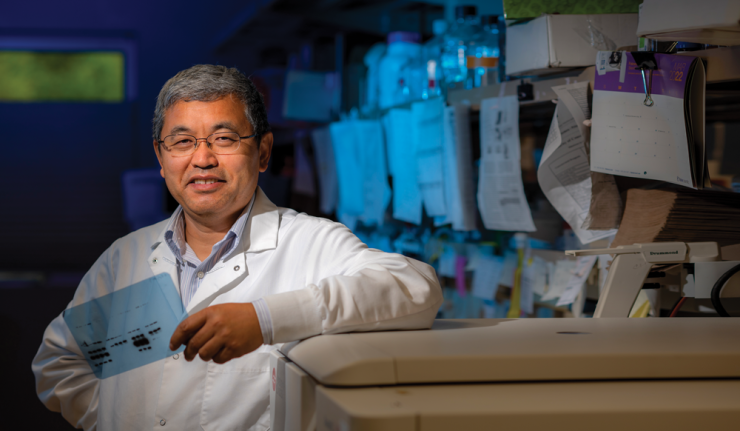
To the trained eye, lens discoloration is an accurate indicator of age, says Dr. Xingjun Fan, aging researcher at the Medical College of Georgia and James and Jean Culver Vision Discovery Institute at Augusta University. It also sets the stage for cataracts as glutathione levels continue to drop and collective UV damage builds, turning the previously pristine then yellowish lens opaque.
Why glutathione production decreases with age has remained elusive. Fan’s National Eye Institute-funded work has uncovered evidence that the enzyme that makes glutathione, called gamma-glutamyl-cysteine ligase, literally gets shorter with time, and the collective impact is less glutathione eventually gets made, something which he thinks is a key event in development of age-related cataracts. His work may make the enzymatic changes a key focus for designing novel anti-cataract therapies.
Fan, who has been focused on the lens for more than a decade, says people have often asked him why he studies cataracts when surgery can already fix them.
“I would tell people: Don’t look at it as just a cataract. Look at it as the aging body. This is a fascinating amino acid peptide in our body,” Fan says of the antioxidant glutathione, which has become a focus for him and his research team in their quest to understand aging.
“It’s highly abundant in your cell system,” he says, found at levels that most other compounds can’t reach, at least while we are young. That’s probably a good thing because cells without glutathione die, he says of this powerful protector from reactive oxygen species, or ROS.
ROS is a byproduct of our body’s use of oxygen. At more normal levels, ROS actually is necessary to stimulate cell signaling pathways, like for our cells to proliferate. But ROS levels increase as body efficiency and function decrease.
Generally speaking, we and our cells become less efficient at pretty much everything as we age, and that includes the powerhouses that provide cells the fuel they need to maintain their function. These mitochondria are big oxygen users that convert glucose to fuel and in the process burn oxygen and give off carbon dioxide and water. With age, they start producing hydrogen peroxide or other free radicals instead of water.
“During the aging process unfortunately that is a common thing in all tissues of our body,” Fan says. “The surge in oxidation can impact our proteins, DNA, lipids, all key elements of our body,” he says. A compounding consequence can be a chronic state of inflammation that again contributes to a host of diseases from Alzheimer’s to heart disease.
“This kind of increased oxidation is tied to chronic inflammation so that is part of inflammaging,” he says, and the focus of a major initiative at MCG and AU as we look toward the next two decades when older adults are expected to outnumber children for the first time in U.S. history. People age 65 and older are expected to number 77 million, while children under age 18 will number nearly 76.5 million by the year 2034, according to the U.S. Census Bureau.
We need balance
“Our body’s biological system needs equilibrium, balance, and if you tip that balance you start having all sorts of problems,” Fan says.
The busy brain feels like an easy mark. The brain is a big oxygen user too and it’s also rich in polyunsaturated fats, liquid fat molecules that are key to the structure and function of neurons and other brain cell types. But when exposed to high levels of ROS that come with age, the fluid fat can literally harden up and your brain tissue stiffens with it. Neuron activity slows. Also, while brain proteins do turn over, that refresh slows with age. Add to this mix, brain cells that are making less glutathione when you could really use more.
Fan has long wanted to look behind the eye at what glutathione was doing or not doing in the important dynamic of the aging brain.
When entrepreneur and philanthropist James Fickel showed interest in and commitment of millions of dollars to basic science research to better understand and ultimately control the aging process in late 2021, opportunity knocked for Fan to peer deeper into the central nervous system.
“He is just unbelievable,” Fan says of the generous support of $759,800 from the James Fickel Alzheimer’s Disease Research Fund for his look into the brain.
Unhealthy connections
Multiple neurodegenerative diseases are caused by the protein aggregation that occurs in aging, Fan says, and there is compelling evidence that ROS plays a key role in initiating and developing Alzheimer’s, a condition in which aging is a primary risk factor.
There is also growing evidence that amyloid beta peptide, the hallmark plaque that accumulates in the brain with Alzheimer’s, is known to produce ROS which, in turn, increases amyloid beta formation. These plaques were first found by Dr. Alois Alzheimer in 1906 with associated symptoms including memory loss, language problems and unpredictable behavior. He also found the neurofibrillary, or tau protein, tangles that tend to follow amyloid beta production. Like a clogged high-performance engine, the performance slips. Eventually neurons die, the brain tissue hardens and atrophies.
Fan has shown that the age-related decline of glutathione in the eye strongly correlates with cataract formation in both his mouse model of glutathione depletion and in aging humans.
In a mouse knock-in model his lab generated where glutathione levels don’t decline, cataract formation is significantly delayed.
 It’s a similar process in the brain where glutathione levels continuously decline as we age and are most dramatically reduced in the brain in Alzheimer’s, Fan says. Some proteins lose function and others “may gain function but a weird function,” he says, as problems like cognitive impairment set in.
It’s a similar process in the brain where glutathione levels continuously decline as we age and are most dramatically reduced in the brain in Alzheimer’s, Fan says. Some proteins lose function and others “may gain function but a weird function,” he says, as problems like cognitive impairment set in.
While there is no question glutathione goes down in the brain, why it goes down there also remains unanswered and Fan is looking at what happens both when he keeps levels up or brings them back up.
He adds that Alzheimer’s is more like abnormal aging. Everything is worse, from the glutathione level drop to the amount of brain shrinkage. Why some people seem immune to these abnormal changes is something that needs to be studied, he says.
“What we propose is during aging, everyone is not equal,” he says. Some people’s brains age must faster because of a worse environment, others fare better.
An aging biomarker
Like the yellowing of our lenses can tell our age, our blood levels of glutathione may one day serve as a biomarker of our aging environment, Fan says, and help explain why some grandmothers are sharp as ever at 95 while others show signs of forgetfulness at 60.
Fan’s lab already has generated a mouse in which the enzyme that makes glutathione, gamma-glutamyl-cysteine ligase, is missing from the forebrain, an area involved in a host of functions like receiving and processing sensory information, thinking and perception and controlling motor function. This FIGSKO mice develops neurodegeneration, particularly in the hippocampus, the center of learning and memory, where the mitochondria that provide power to those neurons, become dysfunctional, and they develop cognitive impairment with age.
They are developing several other research models including an amyloid beta precursor protein transgenic mouse in which they can delete the enzyme that makes glutathione. They also are using human neurons from the hippocampus with and without a so-called Swedish mutation that is proven to increase beta amyloid levels in the brain. Amyloid precursor protein plays an important role in the healthy brain like helping steer neurons to the right place during development. But mutations of this gene can make it destructive as well, as it becomes part of the toxic plaque in the brain with Alzheimer’s.
One of his models is that mouse whose aging is accelerated by reducing glutathione levels. He’s breeding those mice with a standard Alzheimer’s model to look at the impact on behavior, the impact on important brain dynamics like metabolism, how neurons connect and whether they die, something that happens at significantly increased levels in Alzheimer’s versus normal aging. Then, what happens, for example, if they help restore younger levels of glutathione, including mimetics ( or mimics) he has developed. He’ll give the mimetics to each of those models as well to see what brain changes it prompts, including important bottom lines like behavior and neuron connectivity.
“If we understand why glutathione levels keep going down even in normal aging, then we can find a way to intervene and prevent that continued decline,” he says.
They are using these models to better delineate how too little glutathione effects what amyloid precursor protein is producing and, ultimately, on destructive plaque production in the brain. And, the antioxidant’s impact on the function of those cell powerhouses, which in Alzheimer’s can become very good at producing destructive ROS as well, helping create the vicious, destructive cycle. They also are looking at the cognitive and behavioral impact in different models of different levels of glutathione deficiency.
The information Fan’s laboratory is generating because of young philanthropist Fickel’s interest and generosity is allowing his pursuit of federal funding for more findings. And there are many questions to answer.
But while glutathione’s importance is clear, just taking it may not be an answer.
People have long rushed to antioxidant related trials, but they fail miserably, Fan says. “We really need to understand at the molecular level at which stage we should deliver what. We really need to understand what we are doing,” he says, sharing that he doesn’t take the glutathione supplements which are readily available.
An answer may be one or two steps before glutathione, he says, with the enzyme that produces it or even earlier. Scientists at the University of Washington, for example, have a transgenic mouse that overexpresses the gene for this enzyme and it shows positive benefit but we can’t do that with humans, he says of this level of genetic manipulation. “We have to understand what happens even before that, like the signaling that regulates this enzyme,” he says. Or even the step before that.
Or, like probiotics, the reason many antioxidants don’t work may be as simple as not being certain the compounds get where needed to do what is needed.
Either way, what these dramatically reduced levels of glutathione do in the aged and Alzheimer’s brain has to be understood before you know exactly how to target what, Fan says.
In the meantime, he adds, a healthy diet high in foods that are naturally high in glutathione or its precursors, like broccoli, cauliflower, cabbage, bok choy, Brussels sprouts and melons, is always a good idea.
—————-
Box: To donate to Dr. Fan’s research, visit https://mcgfoundation.org/give-now/ and denote fund 8393T, call 706-721-4001 or email philanthropy@augusta.edu