Dr. David L. Mattson
Chair
Physiology
He had just come back from his lab and Dr. David L. Mattson was excited.
Mattson and his former postdoc, Dr. Justine M. Abais-Battad, who came with him to MCG this summer from the Medical College of Wisconsin, had been running through a presentation she was giving the next day.
“It’s just the greatest stuff,” says Mattson.
The new chair of the Medical College of Georgia Department of Physiology is a man who is both collected and exuberant, accomplished and still very curious.
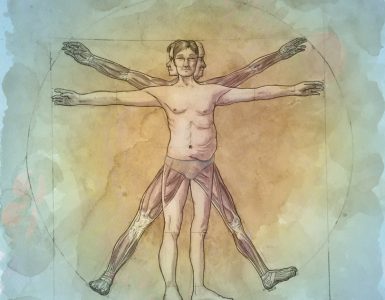
His new administrative focus is to further strengthen an 80-plus year old department whose core mission is understanding how the body works.
His science focus is pervasive hypertension, particularly the role of the kidneys in this major risk factor for heart disease and stroke, and the particular peculiarity of salt sensitivity.
Sensitive to salt
While we have all been told to go easy on the salt, or sodium chloride — good advice, Mattson adds — the reality is most of us are not salt sensitive.
Our bodies don’t make salt, so we have to consume it and one way the kidneys help us retain the valuable commodity is by retaining water, which constitutes the fluid, or plasma, part of the blood.
Our kidneys constantly make decisions about how much salt and water to hold onto, so ideally our blood pressure is keeping us properly perfused from head to toe.
But for probably half of us — at least by the newest definition of high blood pressure which defines normal as less than 120/80 — something is wrong. Most hypertension is called essential or primary, meaning we don’t know the direct cause, likely a direct reason many patients struggle to get and keep their pressures under control.
Somewhere between 30-70% of people who are hypertensive are believed to have what is called sodium sensitivity of blood pressure, says Mattson, Georgia Research Alliance Eminent Scholar in Hypertension, who is working to further clarify who does and how to better address it.
Salt-sensitive hypertension is potent, causing more cardiovascular damage, earlier damage and shorter, sometimes painful, lives as the delivery of oxygen and blood is stymied. Blacks appear disproportionately affected.
“Salt is like a poison to them,” says Mattson. And, like many things in life, its venom creates a vicious cycle of causing some tissue damage which activates the immune response which causes more damage and dysfunction.
The “aggravating” problem was an early, easy sell for Mattson.
Land of lakes, love of science
His father Louis was a geologist in iron-rich northern Minnesota and mother Peggy an elementary school teacher who stopped teaching to raise her own three children. It was a good life, living on a lake in this “Land of 10,000 Lakes,” with plenty of outdoor fun to help compensate for the harsh winters.
He liked school, math made sense to him and he considers science math’s natural partner. Still as a biology major at the University of Minnesota, Duluth, he was not certain what to do with all that. He took a physiology course as a freshman alongside medical students and was taken by how blood cells swell and shrink in different solutions and how the cardiovascular system functions.
As a senior, he saw a poster about a PhD program in biomedical sciences at Wright State University, applied without ever visiting, was accepted and went. While it turned out not to be a great fit, Mattson would come across the work of Dr. Arthur Guyton in the library there. The famed physiologist’s contributions include showing that it was the needs of the body’s tissues, not the heart, that determine how much blood the heart pumps out and helping define the kidneys key role in blood pressure regulation. “He took an engineer’s view of cardiovascular control,” says Mattson.
Guyton was also author of the bestselling Textbook of Medical Physiology, and his work and writing captured Mattson.
Guyton was retiring from the faculty of the University of Mississippi Medical Center about that time, and Dr. Allen W. Cowley Jr., one of his best postdocs, was chair of the Department of Physiology at the Medical College of Wisconsin in Milwaukee, so Mattson applied. He earned his PhD there, did his postdoc studies there and was a faculty member from 1992 until he came to MCG this summer.

When cheaper is better
Who would have thought, that a simple decision to spend less money on rat food, could further fuel his interest.
The Dahl rats are an icon in hypertension research, developed by another icon, Dr. Lewis K. Dahl, chief of staff at Hospital of the Medical Research Center at Brookhaven National Laboratory in New York, who did some of the earliest work looking at the relationship of salt and hypertension. While Dahl and his colleague Dr. R.A. Love would find a steady high salt diet was definitely a factor in hypertension, he would find that, like humans, not every rat would become hypertensive on a high salt diet, which is why he developed a rat researchers could count on.
Flash forward to 2001. While Mattson’s lab has been continuously funded by the National Institutes of Health since 1997, he was looking for a way to stretch those valuable dollars so he decided to switch to some cheaper chow for the Dahl salt sensitive rats.
“It was actually quite a lot of salt,” in both chows, says Mattson. But the rats consuming the cheaper chow did not develop hypertension or the expected kidney damage. The gut reaction was that they would just have to keep buying the more expensive stuff but close behind was the thought this was actually a research opportunity.
While most of us tend to associate cheaper food with less healthy ingredients, Mattson says, in this case it turned out that a whole grain-based chow was cheaper to produce than the standard chow, which takes defined amounts of proteins, fat, carbohydrates and other ingredients and compacts them.
His lab started doing side experiments to figure out what was up, like trying to figure out which specific thing in the more expensive food was causing problems.
Whatever the cause, they found the effect to be a keeper that appeared to start with the rat mothers. In 2014 in the journal Hypertension, Cowley, Mattson and others reported that when generations of the mothers also ate the cheaper grain-based diet, that protection against salt sensitive hypertension appeared to be passed along to their offspring, even when the offspring ate the more expensive, higher fat chow after birth.
The additional twist was the protection held even when the scientists swapped embryos early in the pregnancy so that embryos from mother rats that ate the cheaper diet went into the females who consumed the more expensive diet and vice versa.
Findings, also published in the journal Hypertension this summer, show for example, rats fed the less-expensive grain-based diet were essentially protected from increases in blood pressure; signs of kidney damage like albumin, a main protein of blood, in the urine; and immune cells moving in to the kidneys to cause more trouble. The work also had them saying that salt was clearly not the only dietary component that mattered.
Their newest work indicates that, also like people, the food the rats eat impacts what bacteria are in their gut digesting that food and playing a role in the immune response.
“When we feed these rats these different foods, the bacteria that are in their gut have a completely different profile,” he says. “What we think it does is these different bacteria release different factors, different metabolites that are absorbed into the blood and they can have effects on just about all bodily functions.”
In the case of their focus, high blood pressure and the kidneys, Mattson and team think the metabolites the bacteria release activate the immune system, which amplifies inflammation and disease and that vicious, destructive cycle.
Most recently, Abais-Battad, now an instructor at MCG, did fecal transplants — used in humans to transfer good bacteria from a healthy to an unhealthy person — and found that that didn’t work so well in this scenario but going from the sick to the healthy did make the healthy sick.
The implications could be huge, at least for those with salt-sensitive hypertension, because just switching the diet appears to have such a profound effect on disease.
“Just because you have been eating this bad diet forever, if you make the switch, you likely switch the bacteria and change the pattern of your disease prognosis,” says Mattson.
Knowing if you are salt sensitive is another unresolved dilemma that Mattson hopes to help resolve with a urine or blood test for biomarkers, which indicate your body doesn’t respond well to salt.
In the meantime, the work likely is yet another message to all of us to eat healthy. Recent evidence indicates that even a few millimeters of mercury matter. “We really need to be thoughtful about anything that elevates our blood pressure,” says Mattson.
Elevate physiology, not blood pressure
He prefers that we elevate physiology — the study of how our body does or doesn’t work — and the basic science he considers closest to medicine.
Why he came to Augusta to help do that has more to do with coming here than leaving his academic home of nearly 30 years. He knew about MCG and some of the great physiology faculty, mostly from national physiology meetings. He also is a member of the External Advisory Committee for an NIH Program Project grant, led by Dr. Clinton Webb, Regents’ Professor, pursuing a similar vicious cycle of how high blood pressure causes cell death, which causes more inflammation and hypertension.
He knew the people and place were good, the department history long and solid. He sees the opportunity to build on that as exciting and is talking with faculty now about who to recruit next to best complement them. “It’s a good time.”
Snaptshot: Dr. David L. Mattson
Mattson serves on the governing body of the American Physiological Society as one of nine councilors and has held various leadership roles with the society for 15 years.
Mattson is the American Physiological Society’s 2018 recipient of the Ernest H. Starling Distinguished Lectureship Award for exceptional contributions and lifelong dedication to water and electrolyte homeostasis research.
He is an honored educator, an eight-time recipient of Medical College of Wisconsin’s Outstanding Medical Student Educator Award, who in 2016 was elected to the MCW Society of Teaching Scholars.
Like those who inspired him, he remains thrilled with the opportunity to help educate and inspire, and to date has mentored more than 80 fellows, medical students, graduate students, undergraduate and high school students. One of his current students, MCW PhD student Daniel Fehrenbach came with him to Augusta for his last six months of school.
Mattson loves students’ “absolute” energy and the ideas they conjure up from a class taken or people met. “Students and fellows are really, in my opinion, almost the fuel of a science department,” says Mattson.
He serves as a project leader for an NIH Program Project grant renewal — previously as program director of the grant awarded in 2018 at MCW — elucidating the role of the kidneys in hypertension, including complex interrelationship between factors important in the regulation of sodium excretion; cell growth, proliferation and metabolism; and the immune system. He is principal investigator along with Cowley on a multi-PI NIH grant further exploring the immune system’s impact on salt-sensitive hypertension.
Mattson has served on numerous Special Emphasis Panels and research groups for the NIH and the American Heart Association, respectively, including serving as a member of the AHA Animal Models of Hypertension Writing, Collaborative Science Review and Established Investigator Award Review Groups.
He chaired an NIH Special Emphasis Panel reviewing grant applications for studies of cardiovascular regulation with a focus on the physiology of blood pressure regulation, the pathogenesis of hypertension, and hypertension-related renal and vascular end-organ damage.